Imagine a patient shivering uncontrollably despite being bundled in blankets, or another sweating profusely despite a cool room temperature. These are just some of the scenarios that might arise when a patient experiences ineffective thermoregulation, a common challenge facing nurses across various healthcare settings. As healthcare professionals, our primary responsibility is to maintain a safe and comfortable environment for our patients, and that includes ensuring their body temperature remains within a healthy range.

Image: www.studypool.com
This article will dive deep into the world of ineffective thermoregulation, exploring its causes, manifestations, and most importantly, the nursing care plan that can effectively address this crucial patient need. Our aim is to empower you with the knowledge and skills to provide compassionate and evidence-based care, leading to the best possible outcomes for your patients.
Understanding the Basics: Ineffective Thermoregulation Explained
Ineffective thermoregulation is a state where the body is unable to maintain a stable internal temperature. This can lead to both hyperthermia (excessively high body temperature) and hypothermia (excessively low body temperature). These imbalances can have serious implications, impacting organ function and even leading to life-threatening complications. It’s crucial for nurses to understand the underlying causes and manifestations of ineffective thermoregulation to provide timely and effective interventions.
Common Causes of Ineffective Thermoregulation
- Underlying Medical Conditions: Certain conditions like diabetes, hypothyroidism, and infections can impair the body’s thermoregulatory mechanisms.
- Medications: Some medications, particularly those impacting the central nervous system, can interfere with the body’s ability to regulate temperature.
- Age: Both infants and elderly individuals are more vulnerable to temperature fluctuations due to their immature or declining thermoregulatory mechanisms.
- Environmental Factors: Exposure to extreme temperatures, inadequate clothing, and prolonged immersion in water are common environmental factors contributing to ineffective thermoregulation.
- Surgical Procedures: Post-operative patients often experience a temporary decline in their thermoregulatory abilities due to anesthesia and surgical interventions.
- Trauma or Injury: Severe injuries and trauma can disrupt the body’s temperature control mechanisms.
Recognizing the Signs: Manifestations of Ineffective Thermoregulation
The signs and symptoms of ineffective thermoregulation vary depending on whether the patient is experiencing hyperthermia or hypothermia.
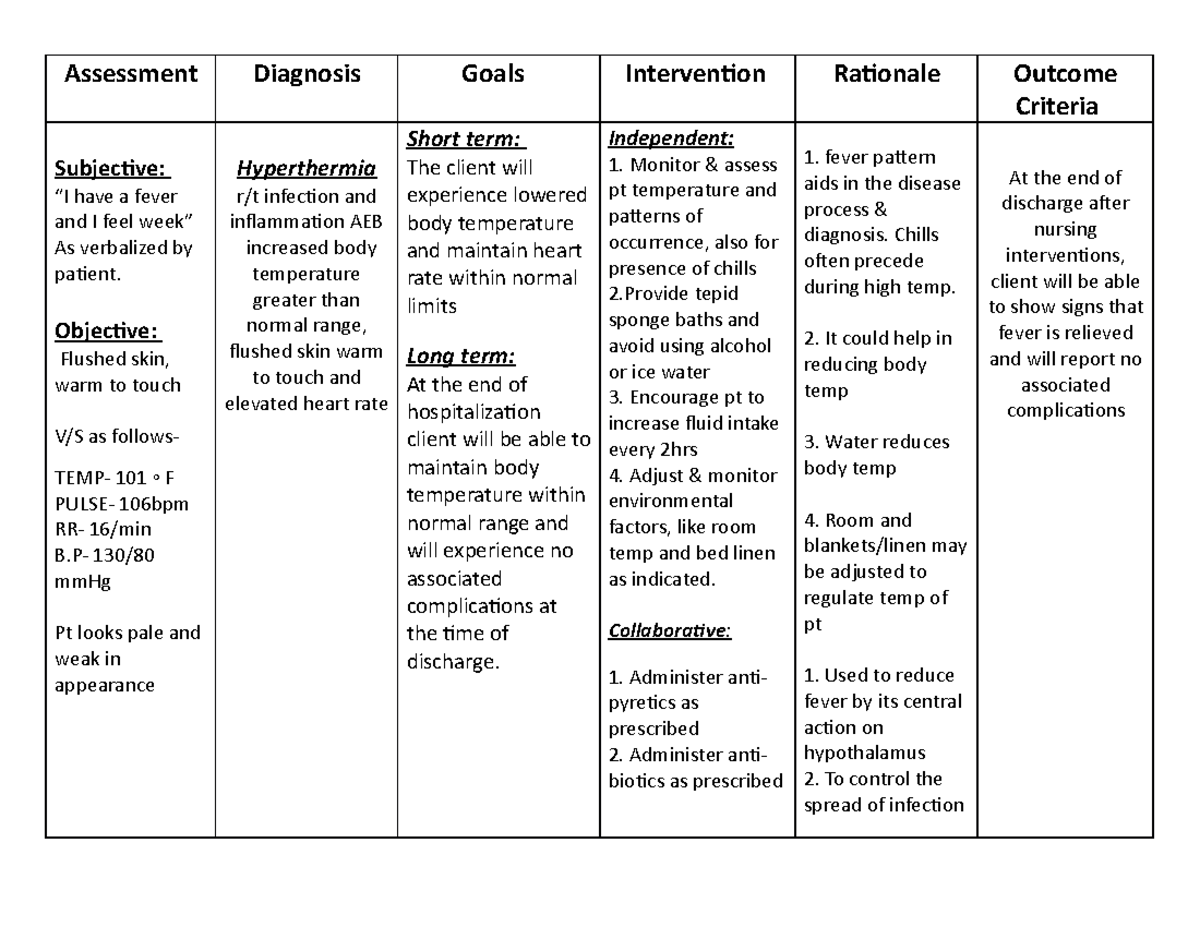
Image: www.studocu.com
Hyperthermia (Elevated Body Temperature)
- Skin: Warm, flushed, or even hot to the touch
- Sweating: Profuse sweating, often accompanied by a rapid pulse
- Breathing: Rapid, shallow breathing, possibly with labored respirations
- Mental Status: Confusion, disorientation, delirium, or even seizures
- Other: Muscle cramps, headache, dizziness, nausea, and vomiting
Hypothermia (Lowered Body Temperature)
- Skin: Cool, pale, or even bluish in appearance
- Shivering: Involuntary shivering, but sometimes absent in severe hypothermia
- Breathing: Shallow, slow respirations
- Mental Status: Confusion, drowsiness, slurred speech, and impaired coordination
- Other: Fatigue, weakness, and a slow pulse
Crafting a Nursing Care Plan: A Step-by-Step Guide
A comprehensive nursing care plan for ineffective thermoregulation is essential to ensure the safety and comfort of our patients. Here are the key steps involved:
1. Assessment: Assessing the Patient’s Thermoregulatory Status
- Temperature Measurement: Take accurate temperature readings using a reliable thermometer, noting the route used (oral, rectal, axillary, etc.)
- Vital Signs Monitoring: Monitor vital signs frequently, paying close attention to pulse, respirations, and blood pressure.
- Physical Assessment: Observe the patient’s skin temperature, color, and moisture.
- Patient History: Gather information about any underlying medical conditions, medications, recent environmental exposures, and surgical procedures.
2. Diagnosis: Identifying the Patient’s Nursing Diagnosis
Based on the assessment findings, a relevant nursing diagnosis can be formulated. Some common diagnoses related to ineffective thermoregulation include:
- Ineffective Thermoregulation: The body’s temperature regulation mechanisms are unable to maintain a stable core temperature.
- Risk for Ineffective Thermoregulation: The patient is at risk for developing ineffective thermoregulation due to underlying factors.
- Hyperthermia: The patient’s body temperature is elevated above normal.
- Hypothermia: The patient’s body temperature is below normal.
3. Outcome Identification: Establishing Patient-Centered Goals
- Maintain a stable body temperature within the normal range.
- Demonstrate an understanding of factors that can influence thermoregulation.
- Implement strategies to prevent further fluctuations in body temperature.
4. Planning: Developing Effective Interventions
Based on the identified diagnoses and desired outcomes, a comprehensive care plan should be developed, including the following interventions:
-
Environmental Management:
- Temperature Control: Adjust room temperature to a comfortable level, using heating or cooling systems as appropriate.
- Adequate Clothing: Ensure the patient is appropriately dressed for the ambient temperature, using blankets or light clothing as needed.
- Avoid Overcrowding: Avoid over-crowding the patient’s space to prevent excessive heat build-up.
-
Pharmacological Interventions:
- Antipyretics: Administer fever-reducing medications (acetaminophen, ibuprofen) as prescribed and monitored.
- Fluid Management: Encourage oral hydration, providing intravenous fluids as needed to maintain fluid balance.
-
Non-Pharmacological Interventions:
- Cooling Measures:
- Tepid Bath: Use a lukewarm bath or sponge bath to lower body temperature.
- Cool Compresses: Apply cool compresses to the forehead, neck, and groin areas.
- Fan: Use a fan to circulate fresh air around the patient.
- Warming Measures:
- Warm Blankets: Use warm blankets to increase body temperature.
- Warm Drinks and Foods: Encourage warm beverages and foods.
- Warm Compresses: Apply warm compresses or heating pads to the extremities.
- Positioning:
- Elevate Head: Elevate the patient’s head slightly to improve air circulation.
- Avoid Restricting Movement: Allow the patient to move freely within safe limits.
- Cooling Measures:
-
Patient Education:
- Thermoregulation Principles: Educate the patient and family about factors that can affect body temperature.
- Symptom Recognition: Teach them how to identify signs and symptoms of hyperthermia and hypothermia.
- Self-Care Measures: Provide guidance on self-care strategies for managing temperature fluctuations.
5. Interventions: Implementing and Monitoring Interventions
- Frequent Monitoring: Continue to monitor the patient’s temperature and vital signs closely.
- Medication Administration: Administer medications according to the prescribed dosage and route.
- Fluid Intake: Encourage adequate fluid intake and monitor for signs of dehydration.
- Environmental Controls: Ensure the patient is in a comfortable environment, adjusting temperature and clothing as needed.
- Continuous Evaluation: Observe the patient’s response to interventions and adjust the care plan accordingly.
6. Evaluation: Assessing Treatment Effectiveness
- Patient’s Condition: Assess the patient’s overall condition, noting improvements or concerns.
- Temperature Stabilization: Monitor temperature readings to document any stabilization or return to within the normal range.
- Symptom Relief: Observe for a reduction in signs and symptoms associated with hyperthermia or hypothermia.
- Patient Education: Evaluate the patient’s understanding of thermoregulation and their ability to implement self-care measures.
Expert Insights: Practical Tips for Nurses
- Early Detection is Key: Maintain a high level of awareness for potential signs and symptoms of ineffective thermoregulation, particularly in vulnerable patient populations.
- Prevention is Powerful: Implement proactive strategies to prevent ineffective thermoregulation, such as maintaining appropriate environmental temperatures, encouraging fluid intake, and addressing any underlying medical conditions.
- Collaborative Care: Work closely with other healthcare professionals, including physicians, pharmacists, and physical therapists, to coordinate care and ensure optimal patient outcomes.
Nursing Care Plan For Ineffective Thermoregulation
Powerful Takeaways: Empowering Nursing Care
Ineffective thermoregulation is a significant patient safety concern that requires vigilant assessment, careful planning, and compassionate care. By implementing a comprehensive nursing care plan, we can effectively address this challenge, promoting comfort and well-being for our patients. Let’s continue to learn, adapt, and collaborate to deliver exceptional nursing care that truly makes a difference in the lives of those entrusted to our care.





