Imagine this: you’re a busy physical therapist, juggling multiple patients, detailed assessments, and a mountain of paperwork. The pressure to meticulously document each patient’s progress feels overwhelming, leaving you little time for the personalized care that truly drives results. Sound familiar?

Image: www.vestibular.today
Fear not! We’re about to dive into a world of efficiency and effectiveness with the power of physical therapy evaluation templates. These valuable tools can transform your practice, streamlining documentation, fostering consistent evaluation practices, and ultimately, contributing to better patient outcomes.
Understanding the Power of a Physical Therapy Evaluation Template
A physical therapy evaluation serves as the cornerstone of patient care, providing a comprehensive foundation for treatment planning. It’s a detailed record of a patient’s initial condition, including their medical history, injury details, current functional limitations, and individual goals.
But the process of gathering and organizing this information can often be time-consuming and prone to inconsistencies. This is where physical therapy evaluation templates step in, offering a standardized framework to ensure thoroughness and accuracy while maximizing efficiency.
Key Components of a Comprehensive Physical Therapy Evaluation Template
A well-structured physical therapy evaluation template will guide you through essential areas, providing a blueprint for consistent documentation. Here’s a breakdown of key components:
1. Patient Demographics:
- Name: This might seem basic, but accuracy is paramount. Double-check spelling and ensure it matches patient identification.
- Date of Birth: Crucial for accurate record-keeping and verifying patient identity.
- Date of Evaluation: Tracks the progress of the evaluation and treatment plan.
- Medical Record Number: Important for linking records and maintaining patient confidentiality.
- Referring Physician: Essential for communication and coordination of care.
- Insurance Information: Ensures proper billing and coverage for services.
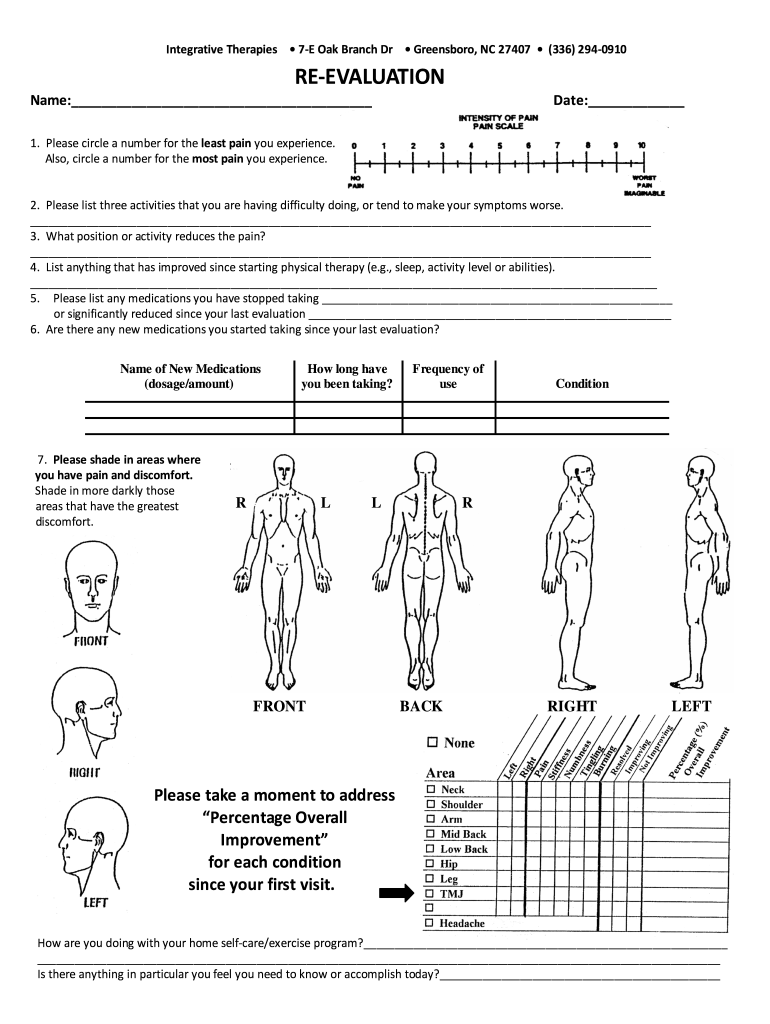
Image: cholonautas.edu.pe
2. History of Present Illness:
This is where you delve into the patient’s current condition, gathering a detailed understanding of their injury or ailment.
- Onset: When did the pain or limitation begin?
- Mechanism of Injury: How did the injury occur? Understand the specific event or activity that led to the problem.
- Location and Character of Pain: Pinpoint the precise location of pain or discomfort and categorize it (e.g., sharp, dull, aching, burning).
- Aggravating and Easing Factors: What makes the pain worse or better? This helps identify potential triggers and guide treatment.
- Previous Treatment: Have they received any prior treatment for this condition? What worked or didn’t work?
- Functional Limitations: How does the condition impact their daily activities, work, or leisure pursuits?
3. Past Medical History:
A thorough review of past medical history is essential for understanding potential contributing factors and guiding treatment decisions.
- Prior Surgeries: Past surgeries can influence current conditions and recovery.
- Chronic Illness: Conditions like diabetes or arthritis can affect overall health and healing.
- Medications: Document current medications, including dosages and frequency.
- Allergies: Ensure patient safety by identifying any potential allergies.
4. Social History:
Social factors play a significant role in recovery. Understanding patient lifestyle can help tailor treatment and set realistic goals.
- Occupation: Does their job involve physical demands?
- Hobbies & Activities: What are their interests and how do they impact their mobility or limitations?
- Living Situation: Who lives with them? Are they able to access necessary resources?
- Living Environment: Are stairs, uneven surfaces, or environmental factors contributing to their limitations?
5. Patient Goals:
Clearly defined goals are essential for successful treatment.
- Short-Term Goals: What specific improvements would they like to achieve in the short term?
- Long-Term Goals: What are their ultimate aspirations related to this condition?
- Functional Status: How would achieving their goals impact their daily living?
6. Physical Examination:
- Observation: Describe the patient’s posture, gait, and any visible deformities.
- Palpation: Examine the affected area for tenderness, swelling, or heat.
- Range of Motion (ROM): Assess the limits of movement in all planes.
- Strength Testing: Evaluate muscle strength in targeted groups.
- Special Tests: Perform tests specific to the condition to determine the extent of injury or dysfunction.
- Neurological Testing: Assess sensation, reflexes, and nerve function, particularly if nerve involvement is suspected.
- Gait Analysis: Observe and document their walking patterns for functional assessment.
7. Evaluation of Functional Abilities:
Assess how the patient’s condition impacts activities of daily living (ADL).
- Bed Mobility: Are they able to get in and out of bed safely?
- Transferring: Can they safely transfer from a chair or toilet?
- Walking: Can they walk independently, with assistive devices, or not at all?
- Stair Climbing: Can they navigate stairs safely?
- Balance: Test their stability and ability to maintain equilibrium.
8. Prognosis & Treatment Plan:
Based on the evaluation results, outline the patient’s projected recovery and a tailored plan.
- Treatment Goals: What specific functional improvements are you aiming for?
- Treatment Interventions: Describe the modalities and interventions you’ll use (e.g., manual therapy, exercises, modalities).
- Frequency & Duration: How often will they receive treatment and how long should the course be?
- Home Exercise Program (HEP): Prescribe specific exercises for home practice to encourage self-management.
- Patient Education: Inform the patient about their condition, treatment plan, and self-care strategies.
- Re-Evaluation Schedule: Schedule follow-up evaluations to monitor progress and adjust the plan if needed.
Benefits of Using Physical Therapy Evaluation Templates:
- Time Savings: Templates streamline the documentation process, freeing up time for patient care.
- Consistency: Templates ensure that all evaluations adhere to a standardized format, promoting uniformity and accuracy.
- Reduced Errors: Templates minimize the risk of overlooking critical information during the evaluation.
- Enhanced Patient Care: Templates guide a thorough assessment, leading to better understanding and more effective treatment plans.
- Improved Communication: Clear and concise documentation facilitates communication with other healthcare professionals.
- Compliance with Regulations: Templates help ensure adherence to relevant regulations and best practices.
Expert Insights & Actionable Tips:
- Customization is Key: While templates provide a valuable framework, don’t be afraid to customize them to meet the specific needs of your practice and patients.
- Technology Integration: Consider using electronic medical record (EMR) systems that offer built-in templates and automated documentation features.
- Train Your Team: Ensure all staff members are well-versed in using and adhering to the chosen templates.
- Regular Review and Update: Periodically review and update templates to reflect evolving practices and evidence-based guidelines.
Physical Therapy Evaluation Template Word Doc
Conclusion:
Physical therapy evaluation templates are a game-changer for modern practices. By embracing this tool, you can simplify documentation, improve the consistency of your evaluations, and ultimately enhance the quality of care you provide. Remember, effective documentation is not just about paperwork; it’s about empowering you to deliver the best possible outcomes for your patients.
Are you ready to streamline your practice and maximize your impact? Start by integrating physical therapy evaluation templates today! Share your experiences and insights in the comments below to help others on their journey towards more efficient and effective care.





