Imagine a persistent urge to urinate, accompanied by a burning sensation, and a feeling of incomplete bladder emptying. These are just some of the uncomfortable symptoms that can signal a urinary tract infection (UTI). UTIs are common, affecting millions of people each year, and understanding the underlying nursing diagnosis is crucial for effective management and patient care.

Image: webapi.bu.edu
A nursing diagnosis for a UTI involves identifying the specific signs and symptoms that the patient is experiencing, as well as assessing their individual risk factors. This process helps nurses to develop a personalized care plan that aims to alleviate symptoms, prevent complications, and promote overall well-being. This article will delve deeper into the various aspects of nursing diagnosis for a UTI, providing insights into the complexities of this prevalent health concern.
Understanding the Basics of Urinary Tract Infections
Before we dive into the nursing diagnosis, it’s important to grasp the fundamentals of urinary tract infections. UTIs occur when bacteria, often from the gut, travel through the urethra and infect the urinary tract. This can involve the urethra itself, the bladder (cystitis), or even the kidneys (pyelonephritis).
Common Symptoms of a UTI
A UTI typically presents with a range of symptoms, and their severity can vary significantly from person to person. Some common signs include:
- Frequent urination: This is often the first sign, as the bladder is irritated and attempts to expel the infection.
- Burning sensation during urination: This is a telltale sign of inflammation in the urethra.
- Pain or pressure in the lower abdomen: This can be a result of bladder irritation.
- Blood in the urine: This can indicate a more severe infection.
- Cloudy or foul-smelling urine: These changes are often indicative of bacterial presence.
Risk Factors for UTIs
While UTIs can affect anyone, certain factors increase the risk of developing them. These include:
- Female gender: Women are more prone to UTIs due to their shorter urethra, which provides easier access for bacteria.
- Sexual activity: Sexual activity can introduce bacteria into the urethra.
- Menopause: Reduced levels of estrogen can affect the balance of bacteria in the vagina, increasing UTI susceptibility.
- Diabetes: High blood sugar levels can make it easier for bacteria to multiply.
- Kidney stones: Obstructions caused by kidney stones can increase the risk of infection.
- Indwelling catheters: Long-term use of urinary catheters can also lead to UTI development.
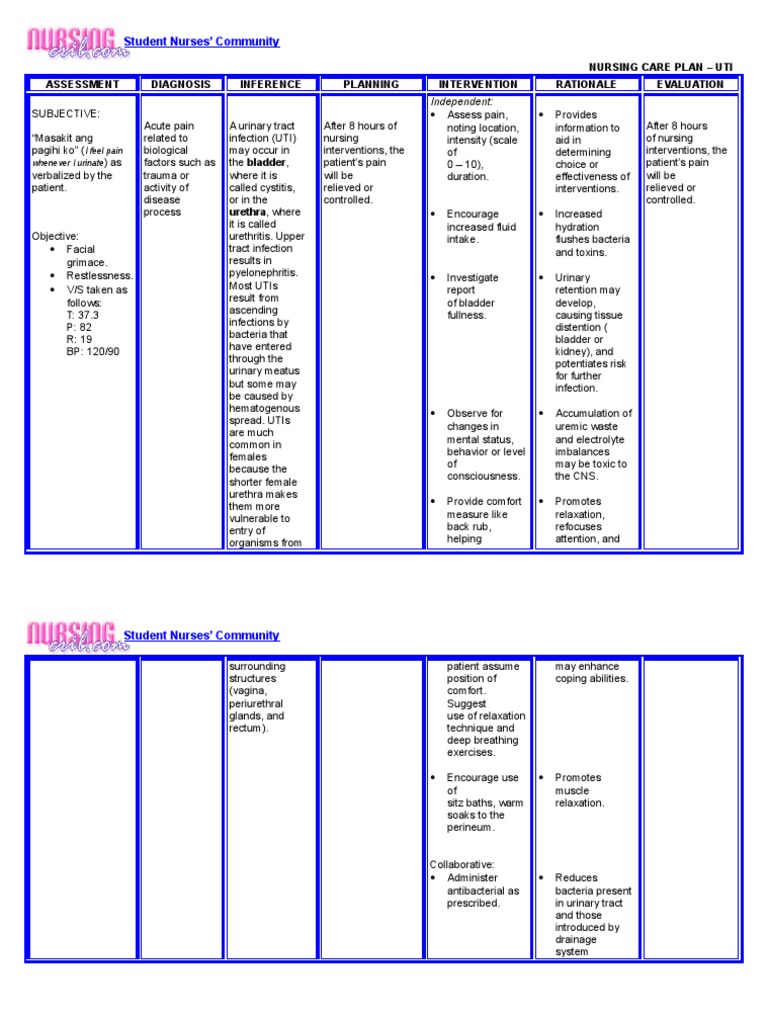
Image: templates.esad.edu.br
The Importance of Nursing Diagnosis for UTIs
The nursing diagnosis process plays a vital role in managing UTIs effectively. It allows nurses to:
- Identify the patient’s individual needs: This involves assessing their specific symptoms, risk factors, and overall health condition.
- Develop a personalized care plan: The diagnosis guides the development of a plan that caters to the patient’s unique circumstances.
- Optimize treatment outcomes: By accurately identifying the problem, nurses can ensure that the patient receives appropriate treatment.
- Promote self-management skills: Nurses can educate patients on ways to prevent future UTIs and manage their symptoms.
Common Nursing Diagnoses for UTIs
Nurses use standardized language to describe patient problems, and for UTIs, several nursing diagnoses are commonly employed. These include:
1. Urinary Elimination, Impaired:
This diagnosis applies when a patient experiences problems with either voiding or controlling urine flow. This can be caused by the pain and discomfort associated with UTI, as well as the underlying infection itself.
2. Pain, Acute:
This is a common diagnosis for patients with UTIs, as they experience pain from the infection and inflammation within the urinary tract. This diagnosis can be further specified by the location of the pain, such as “pain, acute, urinary”.
3. Risk for Infection:
This diagnosis applies when a patient is at an increased risk of developing an infection. In the context of UTIs, this could be due to factors like frequent UTIs, indwelling catheters, or certain medical conditions.
4. Knowledge Deficit: Infection Control:
Patients with UTIs may lack knowledge about infection prevention strategies, such as proper hygiene practices or how to manage symptoms effectively.
5. Anxiety:
The pain, discomfort, and uncertainty associated with UTIs can lead to anxiety in patients. This can be especially pronounced if the patient has experienced UTIs in the past.
The Nursing Process: From Assessment to Evaluation
The nursing process is a systematic approach to providing patient care. It involves five key steps:
1. Assessment:
This step involves gathering information about the patient’s condition, including their history, symptoms, and risk factors. Physical assessment might involve inspecting the skin for signs of dehydration, checking vital signs, and examining the abdomen for tenderness. Nurses also conduct a thorough assessment of the patient’s urinary output, including frequency, color, and any unusual smells.
2. Diagnosis:
Based on the information gathered during assessment, nurses formulate a nursing diagnosis. This involves identifying the specific problem that the patient is experiencing and its potential causes. For example, a patient with pain, frequent urination, and burning during urination might be diagnosed with “Urinary Elimination, Impaired” and “Pain, Acute, Urinary”.
3. Planning:
The planning phase involves developing a course of action to address the patient’s needs. The nursing diagnosis guides the selection of interventions, such as medications, fluids, and patient education on how to prevent future infections.
4. Implementation:
In this phase, the planned interventions are put into action. This could involve administering medications, monitoring the patient’s vital signs, providing comfort measures, and educating the patient on how to manage their symptoms and reduce their risk of future UTIs.
5. Evaluation:
The final step of the nursing process is to evaluate the effectiveness of the interventions and assess whether the patient’s condition has improved. This involves monitoring the patient’s symptoms, reviewing their urinary output, and evaluating their understanding of preventive measures.
Collaborative Nursing Care for UTIs
Nurses play a crucial role in managing UTIs, but it’s important to recognize that they do not work in isolation. Collaborating with other healthcare professionals, such as physicians and pharmacists, ensures comprehensive and effective patient care.
For example, nurses work closely with physicians to ensure the patient receives appropriate antibiotics to treat the bacterial infection. They also collaborate with pharmacists to monitor for potential drug interactions and adverse effects.
Preventing UTIs: A Key Role for Nurses
Nurses play a crucial role in educating patients on ways to prevent UTIs. This involves promoting healthy lifestyle habits and providing guidance on specific strategies to reduce their risk of infection. Some key recommendations include:
- Drink plenty of fluids: Staying hydrated helps flush out bacteria from the urinary tract.
- Urinate frequently: Holding urine can increase the risk of infection.
- Wipe front to back: Proper hygiene practices can prevent bacteria from entering the urethra.
- Wear loose-fitting clothing: Tight clothing can trap moisture and create an environment conducive to bacterial growth.
- Avoid bubble baths and feminine hygiene products: These products can irritate the sensitive skin around the urethra and increase the risk of infection.
Nursing Diagnosis For Urinary Tract Infection
Conclusion: A Holistic Approach to UTI Management
Understanding the nursing diagnosis for UTIs empowers nurses to provide effective and compassionate care to patients. By accurately identifying the signs and symptoms, developing personalized care plans, and promoting preventive measures, nurses play a vital role in managing this common health concern. Through a collaborative approach with other healthcare professionals and patient education, nurses can help patients regain their well-being and prevent future UTIs.
If you’re experiencing symptoms of a UTI, remember to consult with your healthcare provider for diagnosis and treatment. A prompt evaluation and appropriate medical care can help alleviate discomfort, prevent complications, and promote overall urinary health.





