Imagine a patient who presents with confusion, lethargy, and headaches – a seemingly routine scenario for many nurses. However, what if the root of their symptoms lies in an electrolyte imbalance, specifically a low sodium level in their blood, known as hyponatremia? This seemingly simple condition can have serious consequences, making it essential for nurses to be well-versed in its management. Understanding hyponatremia and developing a comprehensive nursing care plan is not only crucial for patient safety but also a testament to the quality of care we provide.
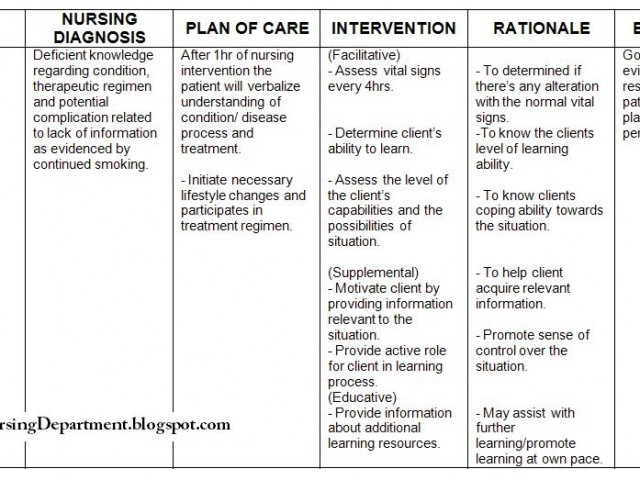
Image: architecturedesign99.blogspot.com
Hyponatremia refers to a serum sodium level below 135 mmol/L, a condition that can result from various causes encompassing water retention, sodium loss, or a combination of both. This condition can be acute or chronic, with severity ranging from mild, leading to subtle symptoms, to severe, potentially life-threatening consequences. This article will delve into the intricacies of hyponatremia, exploring its underlying mechanisms, evaluating the myriad symptoms it can manifest, and, most importantly, crafting a detailed nursing care plan to guide nurses in providing optimal care to patients with this electrolyte imbalance.
Understanding Hyponatremia: A Deeper Dive
Causes of Hyponatremia:
Hyponatremia can be caused by a multitude of factors, with each mechanism contributing to the depletion of sodium in the body. Here are some of the most common causes:
- Water Retention: This is often seen in conditions like heart failure, cirrhosis, and kidney disease, where the body’s ability to excrete water is compromised, leading to an excess of fluid in the body and diluting the sodium levels.
- Sodium Loss: This can occur due to excessive sweating, prolonged vomiting or diarrhea, medications like diuretics, or conditions such as adrenal insufficiency (where the body does not produce enough cortisol, a hormone essential for sodium retention).
- Hormonal Imbalances: Conditions like syndrome of inappropriate antidiuretic hormone secretion (SIADH) can cause the body to retain water, leading to hyponatremia. This can occur due to various factors like lung disease, brain tumors, or even certain medications.
Types of Hyponatremia:
Hyponatremia can be classified based on its underlying cause and the patient’s volume status. The most common classifications include:
- Hypovolemic Hyponatremia: This occurs when there is a loss of both sodium and water, resulting in low blood volume. This is often seen in cases of vomiting, diarrhea, or excessive sweating.
- Euvolemic Hyponatremia: This is characterized by normal blood volume but low sodium levels. It is often associated with SIADH and other conditions involving water retention.
- Hypervolemic Hyponatremia: This occurs when there is an excess of both sodium and water, resulting in an expanded blood volume. This is often seen in patients with heart failure, cirrhosis, or kidney disease.

Image: www.timeofcare.com
Clinical Manifestations of Hyponatremia:
The symptoms of hyponatremia can vary depending on the severity and underlying cause. However, some common presentations include:
- Neurological Symptoms: Confusion, lethargy, headache, seizures, and even coma are common signs of hyponatremia, particularly in severe cases.
- Gastrointestinal Symptoms: Nausea, vomiting, and abdominal cramps can accompany hyponatremia.
- Musculoskeletal Symptoms: Muscle weakness and fatigue can occur, especially in cases of chronic hyponatremia.
- Other Symptoms: Some patients may experience altered mental status, tremors, and even cardiovascular complications like low blood pressure.
Nursing Care Plan for Hyponatremia: A Comprehensive Approach
Assessment:
A thorough assessment is the cornerstone of effective nursing care for patients with hyponatremia. This assessment should encompass the following:
- Medical History: Obtain a comprehensive medical history, focusing on conditions that can contribute to hyponatremia, such as heart failure, kidney disease, cirrhosis, and any history of diuretic use.
- Medication History: Assess the patient’s medication history, including over-the-counter medications, as some can contribute to hyponatremia.
- Physical Examination: Perform a thorough physical examination, paying particular attention to vital signs, neurological status, and signs of dehydration.
- Laboratory Tests: Order serum sodium levels, serum osmolality, and other pertinent laboratory tests to confirm the diagnosis and assess the severity of hyponatremia.
Diagnosis:
The diagnosis of hyponatremia typically relies on laboratory confirmation. The serum sodium level is the primary diagnostic tool. However, the clinical presentation, medical history, and physical examination findings are also essential for formulating a comprehensive diagnosis.
Planning:
Once the diagnosis is confirmed, the nursing care plan is developed to address the specific needs of the patient. The plan should aim to:
- Correct the Hyponatremia: The primary goal of treatment is to correct the hyponatremia by adjusting fluid and electrolyte balance. This is often achieved with intravenous fluids and electrolyte supplementation.
- Address the Underlying Cause: If a condition like heart failure or kidney disease is contributing to hyponatremia, the treatment plan should address these underlying causes.
- Prevent Complications: The care plan should aim to prevent potential complications such as seizures, coma, and cardiac arrest. This may involve monitoring vital signs, neurological status, and fluid balance closely.
Interventions:
Nurses play a vital role in implementing the nursing care plan to achieve the desired outcomes. Some of the key interventions include:
- Fluid Restriction: In cases of euvolemic or hypervolemic hyponatremia, fluid restriction may be necessary to prevent further dilution of sodium.
- Sodium Supplementation: Oral or intravenous sodium supplementation may be used to correct sodium levels, depending on the severity of hyponatremia and the patient’s volume status.
- Medications: Depending on the underlying cause, medications like diuretics or vasopressin antagonists may be used to regulate fluid balance and sodium levels.
- Monitoring: Frequent monitoring of vital signs, neurological status, and serum sodium levels is essential to track the patient’s response to treatment.
Evaluation:
The success of the nursing care plan is evaluated by monitoring the patient’s response to treatment. This includes monitoring the serum sodium levels, clinical symptoms, and the patient’s overall condition. If the patient’s sodium levels remain low, or if they experience worsening symptoms, the care plan may need to be adjusted in consultation with the healthcare team.
Nursing Considerations for Hyponatremia:
Safety:
Monitoring for seizures and other neurological changes is paramount, especially in severe cases. Ensuring a safe environment free of hazards is crucial to prevent injury.
Education:
Educating the patient and their family about hyponatremia, its causes, and the importance of compliance with treatment is crucial for long-term management. Patients should understand the potential triggers of hyponatremia and be prepared to seek medical attention promptly if they experience symptoms.
Self-Care:
Nurses play a vital role in promoting self-care measures for patients with hyponatremia. This includes emphasizing appropriate hydration and dietary management, as well as regular monitoring of symptoms and adherence to prescribed medications.
Nursing Care Plan For Patient With Hyponatremia
Conclusion:
Hyponatremia is a potentially serious electrolyte imbalance that requires a comprehensive understanding and a tailored nursing care plan. From the initial assessment to the ongoing monitoring and education, nurses play a pivotal role in managing this condition and ensuring optimal outcomes for patients. By adhering to the principles outlined in this article, nurses can empower themselves and their patients to effectively manage hyponatremia, promoting patient safety and contributing to the quality of care.





