Imagine the excruciating pain, the chilling fear, and the overwhelming vulnerability that come with a severe burn. This is the reality for countless individuals who have suffered from burns, and it’s a situation where the expertise and compassion of nurses are absolutely crucial. A well-structured nursing care plan is the backbone of effective burn care, guiding nurses through every phase of recovery, from the initial crisis to long-term rehabilitation.

Image: www.scribd.com
This article will delve deep into the intricacies of nursing care plans for patients with burns. We’ll explore the unique challenges posed by this condition, the essential components of a successful care plan, and the vital role nurses play in providing holistic care and fostering patient well-being.
Understanding the Complexity of Burn Injuries
Burns are classified by their depth and extent, impacting the severity of injury and the complexity of recovery. A first-degree burn, affecting only the outer layer of skin, often heals within a few days with minimal scarring. Second-degree burns injure the skin deeper, leading to pain, redness, blisters, and potential scarring. Third-degree burns, the most severe, penetrate all skin layers and even underlying tissues, often requiring extensive skin grafting and long-term rehabilitation.
Key Components of a Nursing Care Plan for Burn Patients
A tailored nursing care plan is fundamental to providing comprehensive and effective care for burn patients. It should address the unique challenges posed by each case, taking into account the patient’s age, overall health, burn depth and extent, and individual needs. The plan serves as a roadmap for nurses, outlining essential steps and interventions to optimize healing, manage pain, prevent complications, and support the patient’s emotional and psychological well-being.
Assessment and Monitoring: The Foundation of Care
The initial assessment is vital for establishing a baseline understanding of the patient’s condition. Nurses meticulously examine the burn site, noting its depth, extent, and any signs of infection. Vital signs are closely monitored, including body temperature, heart rate, and blood pressure, to detect potential complications. Regular pain assessments are conducted using validated pain scales, ensuring that patients receive appropriate pain management.
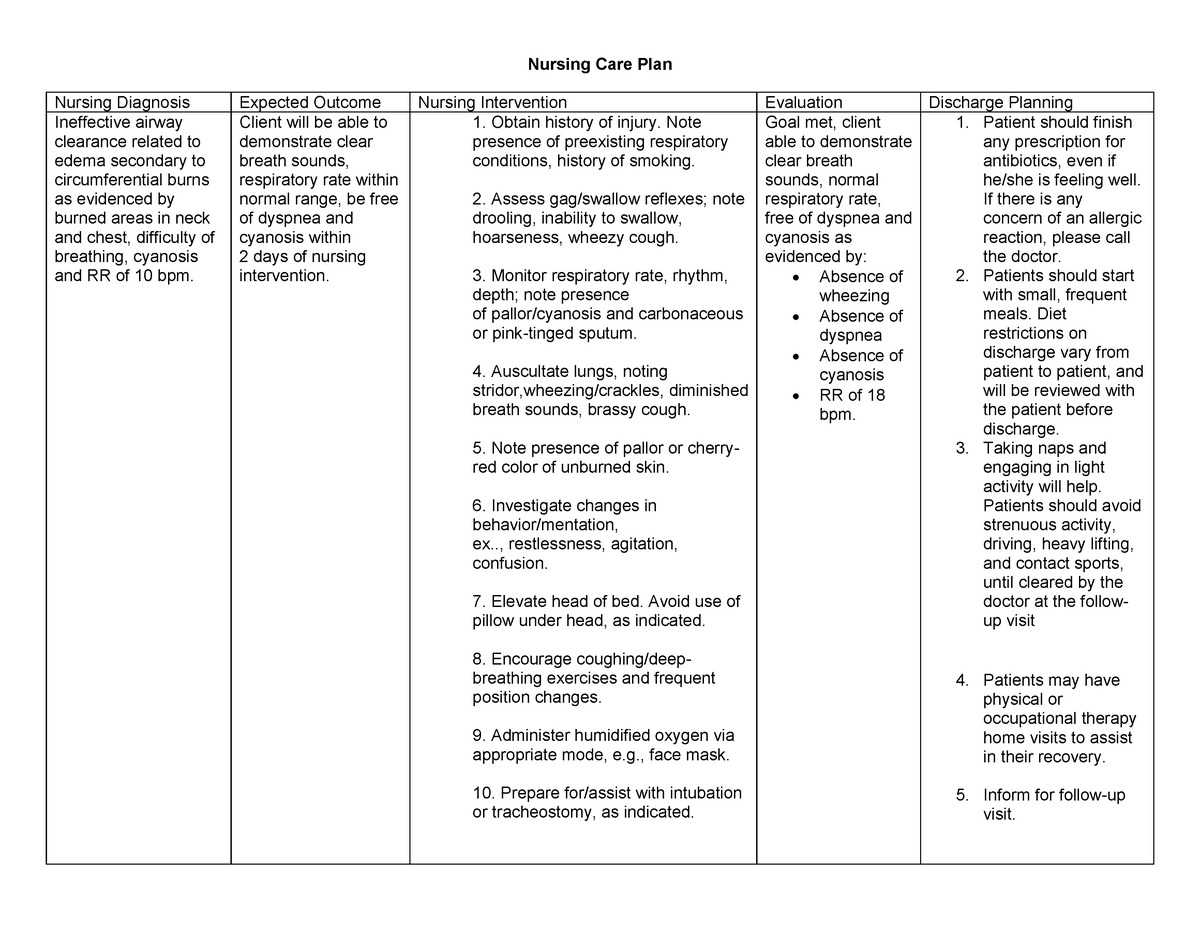
Image: www.studocu.com
Wound Care: Preventing Infection and Promoting Healing
Protecting the burn wound from infection and promoting optimal healing are paramount objectives. Nurses diligently cleanse the wound, remove any debris, and apply appropriate topical medications. They may use dressings to protect the wound from further injury, maintain moisture, and promote healing. In some cases, surgical procedures, such as debridement (removing damaged tissue) or skin grafting, may be necessary for wound closure and healing.
Pain Management: Prioritizing Patient Comfort
Burn pain can be agonizing, ranging from mild discomfort to excruciating agony. Nurses implement a multifaceted approach to pain management, tailoring strategies to each patient’s needs. This may involve administering analgesics, such as opioids or non-opioids, and exploring non-pharmacological methods such as relaxation techniques, massage, distraction, and music therapy. Frequent pain assessments are essential to ensure that interventions are effective and appropriately adjusted.
Fluid and Nutrition Management: Maintaining Body Balance
Burn injuries can cause significant fluid loss, leading to dehydration and electrolyte imbalances. Nurses closely monitor fluid intake and output, ensuring adequate hydration and electrolyte replacement. Nutritional needs are equally critical, as burns increase metabolic demands and can lead to malnutrition. Nurses collaborate with registered dietitians to develop individualized nutritional plans that meet the patient’s specific requirements.
Infection Prevention: Combating the Risk of Complications
Burn wounds are susceptible to infection, which can significantly prolong healing time and increase the risk of complications. Nurses diligently practice meticulous hand hygiene, wear personal protective equipment, and maintain a clean and sterile environment. They also monitor the wound for signs of infection, such as redness, swelling, increased drainage, or fever.
Psychological Support: Addressing Emotional Trauma
Burns can be physically and emotionally devastating, leaving patients with anxiety, depression, body image concerns, and PTSD. Nurses provide compassionate support and understanding, offering a listening ear and addressing emotional needs. They may facilitate access to mental health professionals, support groups, or resources that offer counseling, therapy, and rehabilitation programs.
The Role of Communication and Collaboration: Building a Strong Team
Effective communication and collaboration are essential to providing comprehensive care for burn patients. Nurses work closely with physicians, surgeons, other healthcare professionals, and the patient’s family to ensure that everyone is informed about the patient’s progress, care plan, and any potential concerns. This collaborative approach allows for timely interventions, efficient care coordination, and a smooth transition from acute care to rehabilitation.
Patient Education and Empowerment: Fostering Self-Management
Nurses play a crucial role in educating patients about their condition, care plan, and self-management strategies. This includes providing clear instructions on wound care, medication administration, pain management techniques, and post-discharge follow-up. Empowering patients with knowledge and skills helps them actively participate in their recovery journey and minimize complications.
Promoting Mobility and Functional Independence: The Road to Recovery
Burn injuries often restrict mobility, limiting patients’ ability to perform daily activities. Nurses work closely with physical therapists to develop individualized rehabilitation plans that promote mobility, regain strength, and improve functional independence. This may involve exercises, adaptive equipment, and assistive devices to facilitate walking, dressing, bathing, and everyday tasks.
Scar Management: Minimizing Scarring and Improving Appearance
Scars are a common consequence of burns, often impacting appearance and body image. Nurses play a role in scar management, recommending and applying various topical medications, pressure dressings, or silicone gel sheeting to minimize scarring. They may also refer patients to specialized clinics or programs for more advanced scar management, such as laser therapy or surgical revision.
Long-Term Rehabilitation: Supporting the Patient’s Journey
The recovery journey for burn patients can be long and challenging, requiring ongoing support and rehabilitation. Nurses transition the patient to outpatient settings or support groups, ensuring continuity of care and access to appropriate resources. They may also provide guidance on psychosocial support, vocational rehabilitation, and advocacy to help patients navigate the challenges of reintegrating into society.
Nursing Care Plan For Patient With Burns
Conclusion: A Journey of Healing and Hope
Nursing care plans for patients with burns are essential for delivering personalized, compassionate, and effective care. By understanding the complexities of burn injuries, implementing comprehensive interventions, and providing ongoing support, nurses play a vital role in helping patients heal physically, emotionally, and psychologically. As we learn more about burn care and develop innovative treatments and technologies, the nursing profession remains at the forefront of helping patients rebuild their lives and achieve a sense of hope and well-being.





